What to Do In Case of Needle Stick Injury: Complete Guide
August 6, 2025
Introduction
Needlestick injury is one of the biggest risks to anyone working in the healthcare industry, laboratories, or even those handling medical trash. According to research, doctors account for 73.7% of needlestick injuries, while nurses represent 19.1%.
Fingers are the most frequently injured area. However, despite establishing needle stick injury protocols, these injuries remain prevalent due to unsafe practices and negligence. Therefore, taking immediate steps during these incidents can stop the spread of bloodborne infections, such as HIV, hepatitis B, and hepatitis C, which can have fatal outcomes.
This guide for needlestick injury covers the necessary actions to follow, common infections associated with these incidents, and needlestick injury protocols.
What is a Needle Stick Injury?
Needlestick injuries happen when needles accidentally puncture the skin. These injuries are most common among healthcare workers, doctors, nurses, and emergency personnel but also include those who handle trash.
Although the chances of getting an infection or disease from a needle stick are low, a single pathogen exposure in these injuries can lead to serious infections with life-threatening consequences. However, most needlestick injuries are preventable if you adhere to safety protocols and careful needle-handling techniques.
Importance Of Quick Action After Needle Stick Injuries
Needlestick injuries (NSIs) can potentially impose life-threatening consequences. This is why acting quickly after an injury can drastically reduce the risk of infection and prevent serious health complications.
Even a small puncture from a contaminated needle can introduce infectious fluids into the body. The most common concern is exposure to blood, which can carry dangerous pathogens. Blood exposure significantly increases the risk of transmitting viruses like HIV and hepatitis. Immediate evaluation and treatment can drastically reduce infection risk.
It is where timely medical assessment can be helpful. It can help rule out necessary vaccinations or post-exposure prophylaxis as soon as the infection is detected. Immediate action is also necessary to prevent the spread of bloodborne infections, including hepatitis B, hepatitis C, and HIV.
Overall, immediate actions for needle stick injury include monitoring for signs of infection and performing all necessary blood tests and vaccinations . Hence, establishing a clear post-exposure protocol within healthcare settings can improve outcomes and promote safety. Furthermore, implementing needle stick injury protocols and ongoing education about risks and responses can enhance safety and minimize the impact of these incidents.
Read more: What is Risk Management in Healthcare?
Most Common Infections Caused By Needle Stick Injury
Needlestick injuries (NSIs) carry a significant risk of transmitting bloodborne pathogens, leading to severe infections causing life-threatening diseases. Once you know these possible infections, an immediate intervention can safeguard a person’s health. Some of the most common infections by needle stick injury are:
Hepatitis B Virus (HBV)
The risk of acquiring hepatitis B from a needlestick injury can be huge if the source patient has an active replication of the virus (HBeAg-positive). Vaccination and prompt medical care can minimize the risk of developing clinical hepatitis.
Hepatitis C Virus (HCV)
The likelihood of contracting hepatitis C from an NSI is about 1.8%. Unlike HIV or HBV, there is currently no proven post-exposure treatment to reduce the risk of HCV infection, making preventive measures and swift action all the more important.
Human Immunodeficiency Virus (HIV)
Although the risk of contracting HIV after a needlestick injury is relatively low (approximately 0.3% without post-exposure therapy), it remains a serious concern. There are various factors responsible for the risk of getting HIV, such as the depth of the puncture, whether the needle was inserted into a vein or artery of the previous person, and blood visible on the needle. Immediate intervention within the first 72 hours works best for HIV treatment.
Besides these primary bloodborne viruses, needle stick injury can also expose individuals to other viruses, bacteria, and parasites, including:
- Cytomegalovirus (CMV)
- Epstein-Barr Virus (EBV)
- Treponema pallidum (syphilis)
- Plasmodium (malaria)
The risk of infection depends on the type of needle, the viral load in the blood, and the amount of blood involved. Hollow, large-gauge needles used for procedures like drawing blood or injections into veins and arteries are more likely to transmit infections.
Additionally, accidental exposure can cause localized reactions, including pain, redness, or swelling at the injury site. While, in rare cases, bacteria or fungi present on the needle can cause localized infections.
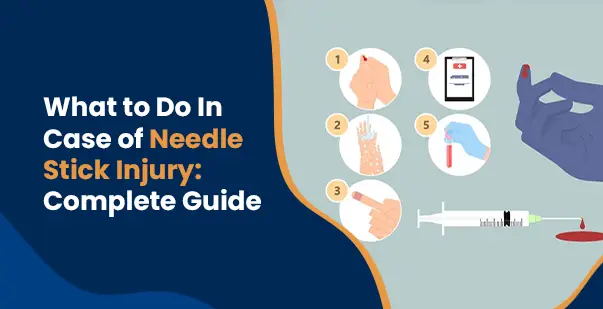
Immediate Steps After Needle Stick Injury
Considering the risks involved in needle stick injury, it’s important to act quickly and take the right steps to reduce the chance of infection. Taking immediate steps will also lower your risk of contracting serious diseases like HIV, Hepatitis B, or Hepatitis C. Here’s what to do if you get stuck with a needle:
-
Wash the Wound Immediately
The first and most important step after a needlestick injury is to clean the wound thoroughly with running water and soap immediately. While antiseptics are not necessary, make sure the area is well cleaned to minimize the risk of infection.
If any body fluid or blood has entered the nose, eyes, or mouth, take a close look and wash it properly with water to avoid further contamination.
-
Find Out The Source Of Needle
Once you’ve cleaned the wound, try to find out as much as possible about the source of the needle. If the needle was used on a patient, you should check whether they are infected with bloodborne pathogens like HIV, Hepatitis B, or Hepatitis C. This information will help guide your treatment and next steps.
-
Seek Immediate Medical Evaluation and Post-Exposure Treatment.
Treat a needlestick injury as a medical emergency and seek immediate care. A healthcare professional will evaluate the severity of the injury and assess the risk based on factors like the depth of the puncture, the location of the injury, and the medical history of the source patient. Depending on the risk level, several treatments are provided to prevent infections:
- A course of antiretroviral medication, HIV PEP (Post-Exposure Prophylaxis), is given within 72 hours of exposure to lower the risk of HIV transmission.
- Hepatitis B vaccination is prescribed immediately to the person who is not already vaccinated.
- Though there is no immediate treatment for Hepatitis C monitoring, the person will be closely monitored for signs of infection.
-
Report the Incident
Many needlestick injuries go unreported, but this can impact your ability to receive proper care. Be sure to notify your supervisor or relevant personnel and follow your workplace’s guidelines for documenting and reporting needlestick injuries.
-
Monitor and Follow Up
After receiving initial medical treatment, continue to monitor the injury site for signs of infection, such as redness, swelling, or pus. Ongoing testing may be necessary to ensure that no bloodborne infections are transmitted.
Preventing Needle Stick Injury
Anyone handling medical waste, needles, or sharps must be trained in preventing needlestick injuries as the first line of defense. Below are the other prevention steps to avoid needle stick injury:
Proper Handling of Needle
One of the primary steps to prevent a needlestick injury is the careful handling of sharp objects like needles. Always use needles with safety features like retractable or shielded needles whenever possible. Never bend, break, or manipulate used needles, as these actions increase the risk of injury.
Proper Disposal of Used Needles
After use, needles should be disposed of immediately in sharps containers designed to prevent accidental injury. Never dispose of needles, syringes, or blades in regular waste bins, as this can be risky to others who may come into contact with them.
Safe Recapping Procedures and Surveillance Programs
Safe recapping procedures must be in place in situations where recapping needles is necessary. Recapping should always be done with the assistance of mechanical devices, never by hand. In addition to safe recapping, surveillance programs should be established to track and monitor needlestick injuries.
Needle Stick Injury Protocols and Regulatory Guidelines
Needlestick injury protocols are enforced by OSHA to reduce occupational exposure to bloodborne pathogens, specifically to prevent the risks posed by bloodborne pathogens. The key regulations by OSHA standards include a few important elements, such as employers must establish exposure control plans detailing the steps to prevent and manage potential exposures to bloodborne pathogens. It mentions that all human blood and certain body fluids should be treated as if they are infectious, regardless of the perceived risk.
Needlestick injury protocols mandate that workers must use personal protective equipment (PPE), such as gloves, masks, and other protective gear. These gears can avoid direct contact with blood or other potentially infectious materials (OPIM). Another important protocol is that affected workers must be provided with appropriate medical evaluation and follow-up care after an exposure incident. Finally, it is a must that employers offer vaccination against Hepatitis B to all employees who are at risk of exposure.
Employer Responsibilities Under OSHA’s Needlestick Injury Standards
Under the OSHA guidelines, any employer whose employees may come into contact with blood or OPIM is required to comply with these standards. This includes not just healthcare settings but also non-healthcare industries where exposure may reasonably occur, such as emergency response and waste management.
Several other roles of employers regarding needlestick injuries are regularly updating the Exposure Control Plans to reflect new technologies and procedures that reduce the risk of injury. Maintaining a Sharps Injury Log to record all incidents involving needles or sharp objects also comes under the employer’s responsibility. This log helps track patterns and allows employers to implement additional safety measures as needed.
Read more: Medical Asepsis vs. Surgical Asepsis: What is Aseptic Technique?
Key Takeaways on Needle Stick Injuries
Needle stick injuries are common in the healthcare industry. They should not be taken lightly due to the serious health issues they can cause. The care provider can get bloodborne infections such as HIV, Hepatitis B, and Hepatitis C, along with other fatal diseases due to contamination of needles. However, taking immediate and informed action following needlestick injury protocols can prevent these health complications.
Employers can significantly reduce workplace risks by strictly following safety measures and needle stick injury protocols. Additionally, continuous training, adhering to protocols, and maintaining best practices for handling needle stick injuries can decrease the likelihood of these incidents.
Read More: Infection Control Course For Caregivers





